It took me over ten years to get to the root of my chronic back pain and be rid of it permanently.
These days, it’s not chronic and the pain is gone.
I’ve been pain-free for the last five years and I know the pain will not come back.
It’s true, I may have a twinge every now and then but as soon as it appears, I notice it, I laugh at it, and it disappears.
Why?
Because now I understand the pain … and myself.
I promise that if you read this long article to the end, you’ll understand your pain from a new and powerful perspective.
This article will be the beginning of your own healing journey.
Disclaimer: This article is for blogging purposes only. It is not meant to treat or diagnose any disease you may or may not have. For medical advice, treatment and diagnosis please see your doctor or a licensed medical professional.
Table of Contents
My Back Pain Story
I’ve suffered from back pain for most of my adult life.
Pain which often lasted for months.
I couldn’t get out of bed, couldn’t sleep, couldn’t walk, couldn’t go to the loo, couldn’t do bloody anything!
I put my dreams on hold a number of times due to back pain.
Pain governed my whole existence.
It was no life.
No meds even touched the pain.
Excruciating, debilitating, paralysing pain.
I tried everything—physiotherapy, osteopathy, massage, acupuncture, yoga, pilates, swimming, meditation, stretching, breathing…
… Sticky patches, tiger balm, TENS machines, back stretchers, hot water bottles, ice packs, Epsom salts, turmeric tablets, magnesium, ginger and all sorts of supplements…
… and CBD oil? I didn’t know about it back then.
And, yes, I slept on my side with a pillow between my legs, or on the recliner or the settee when I couldn’t make it to bed.
Anyway, after a couple of hours, I’d be awake with horrendous back spasms again!
It was time for an MRI.
“There you go. That’s the cause of your pain, Angelos”.
A slipped disc at L4/L5 region.
My pain intensified after the diagnosis.
Now it was not only lower back pain but also pain in my right hip and leg.
Was I ready for surgery?
The surgeons were ready. I saw more than one of them.
I wasn’t ready.
I felt something was not quite right with that slipped disc story.
If the disc had indeed slipped, how come the pain wasn’t constant for all those years?
A disc certainly doesn’t move around your spine.
I was looking for clues like Sherlock Holmes.
A doctor once said to me, “I don’t know how this slipped disc’s giving you the pain you’re talking about. If you saw my MRI, you would think a double-decker had run over me — but I don’t have any pain”.
So, if it was not the slipped disc, what was causing the problem?
Lance, my osteopath, always said: “Sciatica is only the symptom, not the root cause. Medications treat the pain, i.e. the symptoms. The problem is the stiff joints and muscles that create inflammation which in turn create the pain”.
He was right, but, what was causing the stiff joints and muscles in the first place?
Difficult Life Decisions
In 2013, I was probably going through my worst flare-up.
Back then I worked for Barclays Capital and made a lot of money but I felt unhappy with my job.

My family, girlfriend, friends—they all thought I was nuts every time I said I’d quit my job.
It was too much emotional pressure, coming not only from others but also myself.
Getting into investment banking was always a dream for me and I fought hard to get there.
However, when I built the castle, I couldn’t live in it and I knew I had to pull it down.
I turned on myself, experiencing anger for poor decisions I had made in the past. What if I had done this instead of that? Would things be different now?
I was suffering from stress and anxiety and on top of this there was the back pain.
Could it have been that the stress and anxiety were causing the back pain?
I’ll explain more later but for now, let’s look at the science and rule out first what’s NOT creating the pain.
Lie #1 – Herniated Discs Cause Back Pain
There IS NOT a single study in medical literature that proves that spinal “flaws” such as the following cause back pain:
- arthritis
- scoliosis
- disc degeneration
- stenosis
- bulging discs
- herniated discs
Yes, you heard it right.
Herniated discs and disc degeneration disease (DDD) are not responsible for your back pain.
Research has shown that the cause of most low back pain is unknown. Current tests cannot identify a pathological cause for the pain in over 85% of cases.
That is, in over 85% of cases, even when the most extensive testing is conducted, no clear cause can be established.
For this reason, such low back pain is now usually termed non‐specific low back pain.
Study #1 – Healthy Pain-Free People Have “Bad” MRI’s
Waleed Brinjikji et al published a study in which they analysed the MRI’s of 3110 people who never experienced back pain or any symptoms.
They found that a few people from all age groups had disc degeneration and abnormal MRI’s but didn’t have back pain.
The researchers concluded:
Imaging findings of spine degeneration are present in high proportions of asymptomatic individuals, increasing with age. Many imaging-based degenerative features are likely part of normal ageing and unassociated with pain.
Here’s the table with their findings:
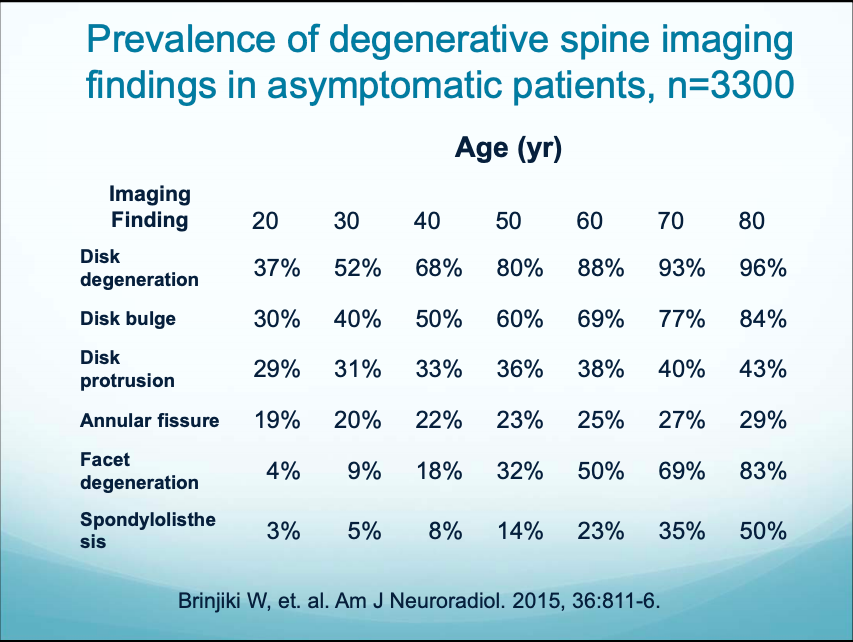
As shown above, if you take healthy 40–year–olds and you give them MRI’s, 68% of them have disc degeneration.
Unbelievable!
Almost 7 out of 10 healthy 40–year–olds have disc degeneration completely pain-free!
If you take completely healthy, pain-free 30-year-olds who never complained about back pain, 40% of them have disc bulges in their MRI’s.
And if you look at healthy people aged 60+, the majority of them have spine flaws but no back pain.
So, how come all the spine flaws didn’t mess around with the spinal nerves of these people?
Study #2 – Stenosis May Be Good for You!
Spinal stenosis is a narrowing of the spaces within your spine, which can put pressure on the nerves that travel through the spine. Spinal stenosis occurs most often in the lower back and the neck.
A 2014 spinal stenosis study by Pekka Kuittinen, et al. in BMC Musculoskeletal Disorders showed that people with moderate stenosis experienced more pain than sufferers with more severe stenosis.
WHHHAAAATT???
There was no correlation between the stenosis on the MRI’s and back or leg pain.
In the discussion section of the study, it states,
The main finding of our study was that there is no linear correlation in the radiological degree of severity of LSS (Lumbar Spinal-Canal Stenosis) and clinical findings.
In contrast, according to the visual evaluations of the central canal LSS, leg pain measured by VAS (Visually Assessed Severity) was higher in the moderate stenosis group than in the severe stenosis group.
Isn’t it amazing what these guys found?
Not only did the stenosis NOT cause the pain but the worse the stenosis looked in the MRI’s, the less pain the people were in, and the longer they could walk without pain.
But why is that? The study says,
One possible explanation to our apparently paradoxical findings
could be the decreased lumbar spine instability in patients with advanced facet joint hypertrophy and large end-plate osteophytes, which in turn would provide pain relief and allow higher walking capacity.
Accordingly, degenerative hypertrophy could be a protective mechanism against the disc degeneration typically found in patients with advanced age.
So, the “spinal flaws” that the doctors blame for back pain may actually be preventing the pain rather than causing it!
* Subscribe to receive my tips on chronic pain relief straight to your inbox *
Study #3 – Your Disc Bulges or Protrusions are MRI Coincidental Findings!
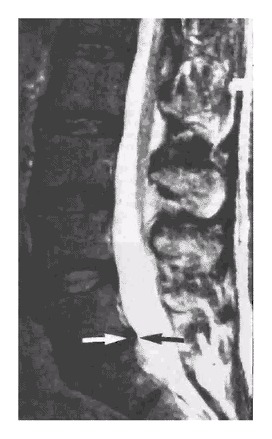
A study by Maureen Jensen in 1994 concluded that,
On MRI examination of the lumbar spine, many people without back pain have disc bulges or protrusions but not extrusions. Given the high prevalence of these findings and of back pain, the discovery by MRI of bulges or protrusions in people with low back pain may frequently be coincidental.
Note: The study was not conclusive when it comes to extrusions because this only applied to a small number of the people in the study. Those few people were asymptomatic too.
The lumbar region of the spine is what we often call the lower back which contains the 5 vertebrae L1-L5 and the spinal discs between the vertebrae.
Here are two MRI’s from the study showing a disc protrusion and a disc bulge in two young women with no back pain.
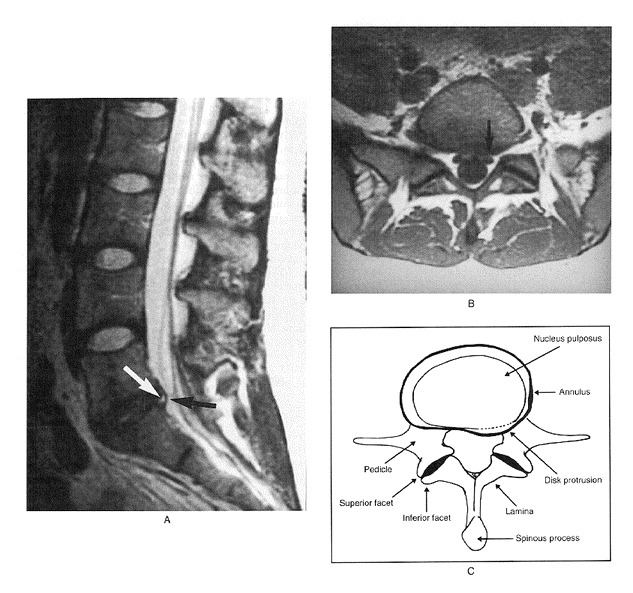
In the discussion section of the study, it states that only 36% of those examined had a normal disc at all levels,
We found a high prevalence of abnormalities in the lumbar spine on MRI examination of people without back pain.
Only 36% of those examined had a normal disc at all levels.
About half had a bulge at at least one intervertebral disc, and about a quarter had at least one disc protrusion.
Given the high prevalence of back pain in the population, the discovery of a bulge or protrusion on an MRI scan in a patient with low back pain may frequently be coincidental.
Therefore, the clinical picture should be correlated with the MRI results.Abnormalities of the lumbar spine by MRI examination can be meaningless if considered in isolation.
Conclusion: An MRI on its own says nothing about your back pain.
Lie #2 – Surgery Will Fix your Back Pain
Professor Howard Schubiner says that “several studies have found no difference in long–term outcomes between surgery and conservative forms of therapy, including physical therapy, observation and exercise”.
I couldn’t believe my eyes when I dived into all these medical studies.
Here are five of them.
Study #1 – Surgery for Sciatica is not Effective in the Long Term
A study published in the New England Journal of Medicine showed that 1-year outcomes for sciatica patients who had surgery were no better to those who received conservative treatment.
Relief was twice as fast in the short-term for those who had surgery but after a year, everyone was in the same boat again pain-wise.
Within a year the test scores which measure the relief from leg pain were practically the same.
Surgery is seen as a magic pill.
Patients expect surgery to put an end to their sciatica forever.
“Could there be anything more powerful than surgery?”, you may ask.
Study #2 – Surgery May Give you Some Relief for … 4 Years!
An award-winning 10-year study on Lumbar Disc Herniation showed that although those who had surgery experienced more relief in the 1st year, the results of surgical and non-surgical treatment were no different after four years.
Study #3 – Microdiscectomy for Disc Herniation … 2 Years of Relief Tops.
Another study published in 2008.
Same story:
There were no clinically significant differences between the groups in leg or back pain intensity, subjective disability, or health-related quality of life over the 2-year follow-up, although discectomy seemed to be associated with a more rapid initial recovery.
Not only that, but the short-term sciatica benefits were only modest according to the study.
Is there a pattern here?
Is short-term relief resulting from surgery real or more of a placebo type of thing?
Study #4 – Spinal Fusion is NOT Effective in the Long Term
Brox et al (2010) did a 4-year follow-up of patients to compare surgical versus non-surgical therapy in the treatment of chronic low back pain.
The study included some patients who had previous surgery for disc herniation while others had no previous spinal surgery. Of the 124 patients, 66 were assigned to the surgical group and 58 to the non-surgical group.
The study showed that,
Lumbar fusion was not superior to cognitive intervention and exercises at relieving back pain, improving function and return to work at 4 years.
Study #5 – People with Herniated Discs Do not Need Surgery
Another study called Back Surgery – Who Needs it? concludes:
Patients with major motor deficits need surgery, as do some with major spine trauma. For these patients, surgery may preserve life or function. Absent major neurologic deficits, patients with herniated discs, degenerative spondylolisthesis, or spinal stenosis do not need surgery, but the appropriate surgical procedures may provide valuable pain relief.
In other words, yes, surgery is absolutely necessary when you’ve got fractures, tumours, inflammatory conditions, or severely herniated discs with evidence of nerve damage, but not for everyone who complains about back pain.
Study #6 – Spinal Fusion for Low Back Pain is Controversial!
A study on the efficacy of spinal fusion done by Eugene Carragee at Stanford showed that,
Fusion surgery appears to offer only limited relative benefits over cognitive behavioural therapy and intensive rehabilitation in randomised control trials of surgical vs. non-operative care.
And their conclusions are even more interesting…
Regardless of the technological advances for intervention, the central question behind any of these strategies however remains.
In patients with common degenerative findings alone, why are some doing very well, some are minimally affected with common backache and others severely incapacitated from all common daily activities?
The diagnosis of low back pain may be a larger problem than choice of intervention.
If much of the severe LBP illness associated with only minor changes of the lumbar spine is, in fact, primarily a function of a generalized pain intolerance, or is an expression of psychological illness such as depression or anxiety, or is secondarily driven by compensation issues,
dysfunctional social adaptation or poor coping skills, little effect will be seen by intensifying efforts to eradicate local, benign pain processes in that subgroup.
More Highlights from the Stanford Study
Here are some more enlightening facts from the same study that hopefully will change the way you see your back pain.
- There is poor correlation between MR findings of spinal degenerative changes and symptoms in adults.
- Most people function well despite significant and progressive spinal degenerative changes.
- The cause of serious LBP illness in the absence of serious spinal diseases such as instability, infection or neoplasm is not well understood and nonstructural factors such as central pain intolerance, psychological distress, social and economic issues of compensation and participation, appear to act as co-morbidities to LBP illness impairing recovery.
- In RCTs of surgical vs. non-operative care, lumbar fusion surgery for common degenerative changes appears to offer only limited relative benefits over intensive rehabilitation. Cohort studies of highly selected subjects have somewhat better outcomes.
- Artificial disc replacement has approximately the same outcomes as fusion in short-term studies but the long-term risks of prostheses placement in relatively young patients remains a concern.
Other Risks and Downsides of Surgery for Back Pain
All the previous studies haven’t taken into account the risks or complications that all surgical operations have.
These risks are small but still, why would you have an operation if it’s not necessary and long term relief is not guaranteed?
What about recovery from anaesthesia?
What about the costs?
What if the operation date the NHS has given you is five, eight, ten months down the line? A few people decide to go private and the costs can go from £3K up to £15K or more.
Lie #3 – Nerve Block Injections for Back Pain Relief
There are numerous studies showing that the benefits of nerve block injections for back pain, are only short-lived if indeed there are any.
Injections Have a Moderate and Only Short-term Effect
A systematic review of nonsurgical interventional therapies for low back pain provided fair evidence that epidural steroid injection is moderately effective for short-term (but not long-term) symptom relief.
Another systematic review of the efficacy of injections for low back pain and sciatica concludes:
The best studies (those with the strongest conclusions) showed inconsistent results of epidural steroid injections. The efficacy of epidural steroid injections has not yet been established. The benefits of epidural steroid injections, if any, seem to be of short duration only.
It’s not your fault if they’ve convinced you that surgery or injections are the solutions to your chronic back pain.
It’s not your fault if your back pain gets worse when you find that none of that worked for you.
Lie #4 – Opioids Can Help with Chronic Back Pain
The medications for back pain relief fall into one of the following categories:
- Non-opioid painkillers – such as paracetamol or aspirin. Some of these are available over the counter from pharmacies and supermarkets. Others may need a prescription.
- Anti-inflammatory drugs – such as ibuprofen or naproxen. These are also known as non-steroidal anti-inflammatory drugs or NSAIDs. Again, some of these can be bought over the counter, and some need a prescription.
- Compound painkillers – this is when two different drugs are combined into one, aka “combos”. This could be a painkiller with an NSAID or an opioid painkiller with a non-opioid painkiller. An example is co-codamol, which combines paracetamol with codeine.
- Opioid painkillers – such as codeine, tramadol, dihydrocodeine, tapentadol, oxycodone, buprenorphine, fentanyl, methadone and morphine. These are the strongest type of painkillers and are only available on prescription.
Is opioid prescription in the UK out of control?
An article in The Times says,
Britain’s opioid epidemic kills five people every day and is hurtling towards a US-style crisis. In the US, super-strength painkillers have killed more than 91,000 people in the past two years.
The Office for National Statistics says that since 2006, over half of all drug poisoning deaths every year involved opiates.
An extensive study that analysed opioid prescriptions and usage in Britain between 1998 and 2018 says,
There is a call for greater monitoring of opioid prescribing in the UK, particularly of strong opioids in chronic pain, for which there is little evidence of clinical benefit.
Between 1998 and 2016, opioid prescriptions increased by 34% in England (from 568 per 1000 patients to 761 per 1000). After correcting for total oral morphine equivalency, the increase was 127% (from 190 000 mg to 431 000 mg per 1000 population).
So, the prescribed dosage has increased by 127% over the last twenty years.
What’s going on? This is madness!
But “I’m constantly in pain, what am I supposed to do?”, you may ask.
Well, this is what the Faculty of Pain Medicine of the Royal College of Anaesthetists says about opioids:
There is no evidence for the efficacy of high dose opioids in long-term pain.
Short-term efficacy does not guarantee long-term efficacy.
Data regarding improvement in quality of life with long-term opioid use are inconclusive.
The NHS website states clearly:
There is little evidence that opioids are helpful for long-term pain.
The use of OTC pain killers (those that don’t require prescription), also shows an upward trend.
Pain relief OTC medication was worth £628m in 2019, increasing 9.3% in value compared to the previous year.
Don’t Tell me I’m Imagining the Pain!
The pain is 100% real.
You’re not imagining the pain.
Although I haven’t given birth (!), mums have told me it’s worse than giving birth.
You wouldn’t wish this pain on your worst enemy.
I’ve been there.
I feel for you and I can appreciate the pain you’re suffering.
Let me tell you this:
- It’s OK if you moan 24/7, swear, cry, get angry at yourself and the whole world.
- It’s OK if you hate people for enjoying their weekends while you’re drugged up and at home in agony.
- It’s OK if you’ve been off work for weeks or thinking of filling in PIP forms.
- It’s OK if you hate the NHS for getting an operation date 10 months down the line.
- It’s OK if you hate Covid-19 for not being able to see a GP and getting a telephone diagnosis.
Because, let me say it again:
The pain is real.
When someone told me it was all in my imagination while I was in excruciating pain, I told them to f*** off.
What I couldn’t see was that the pain was emotional, neurological, brain-induced pain rather than physical pain.
Lie #5 – Pain is Pain
Not all pain is the same.
If “pain is pain”, treatments may be designed to reduce the pain or to help patients cope with the pain.
This practice blurs the line between the two major causes of chronic pain:
- inflammatory pain due to ongoing physical injury, tumour, fracture (i.e., nociceptive pain), or due to nerve damage (i.e., neuropathic pain)
- brain-induced pain (i.e., neural pathway, centralized, psychophysiologic, or psychosomatic pain).
So, What Causes the Bloody Pain?
The chronic pain community is full of hard-working, conscientious, and extremely empathetic people.
Nice people who strive to support each other and truly feel for someone else’s pain too.
People who want to be good—good fathers, good mothers, good sons and daughters, good friends, good people to society—pushing, pushing, pushing to do the right things.
People who are heroes and want to keep everyone around them happy even when they’re experiencing horrendous pain.
People like us.
You may ask, “what does all that have to do with pain”?
Well, in the process of trying to be perfect, you may lose sight of your own needs, who you are, how you feel, and what you want from life.
This can develop into an unconscious internal struggle within—negative emotions, anxiety, anger, fear, sadness, resentment.
Let me say that again: This struggle is often unconscious and repressed.
And it can often be so unbearable that it takes the form of physical pain.
I’m not the one who discovered this.
Dr Sarno, MD was a pioneer who gave the name Tension Myositis Syndrome (TMS) to pain that’s caused by repressed emotions.
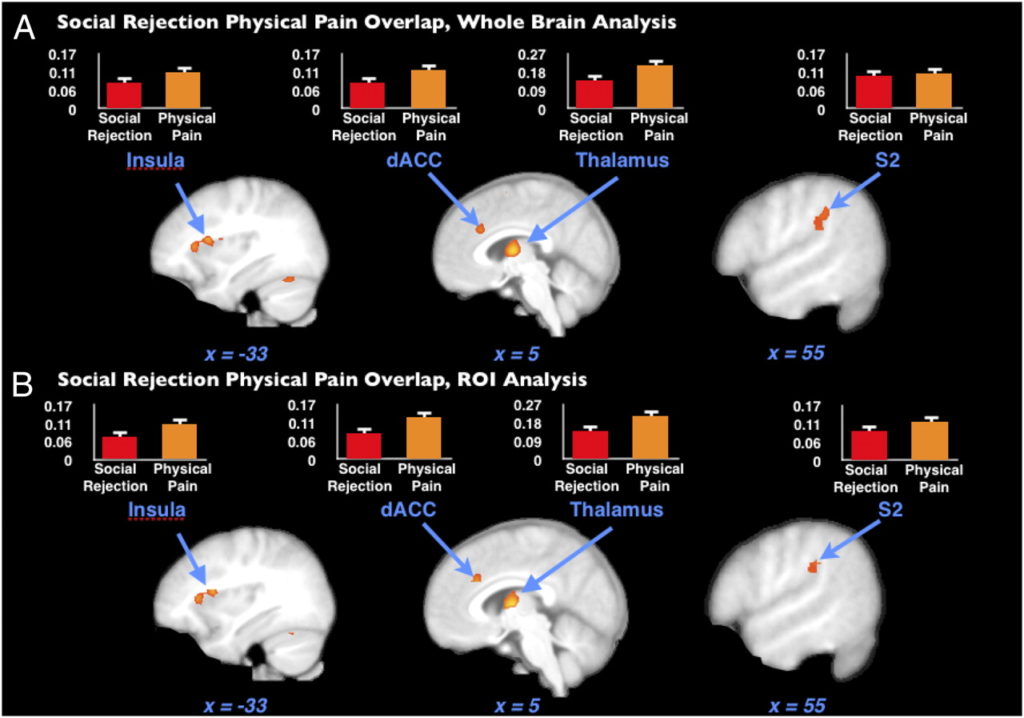
Neuroscience has shown that when someone suffers emotionally, parts of the brain that are activated are identical to those that are activated when they get a physical injury.
Here’s a picture from one scientific study proving that social rejection and physical pain overlap on a neural level.
Your back doesn’t send “pain signals” to your brain.
All sensations, including those associated with severe pain, are electrical signals which go to your brain through your nervous system.
It’s then the job of your brain to encode and interpret those signals and activate a danger-alarm mechanism if necessary.
When you put more pressure on yourself, you have a greater tendency to activate this mechanism.
And as I said earlier, not all pain is emotional.
People have accidents and end up with a broken pelvis, hip, spine, wrist, etc.
At other times, there is clear nerve damage that can be easily seen in an MRI.
However, if you have pain that moves around your body, then disappears and suddenly returns, or you’ve had a couple of operations and it’s still there, your pain may not be injury-induced but brain-induced, neural pathway pain, neurological pain.
There is no disease that gives you back pain when you wake up in the morning, and gets better through the day. So, at 5 pm you’re all of sudden pain-free, but it comes back at night with pain in the shoulders.
There is no disease that does this.
But it’s possible to experience that because neuropathways can turn on and off.
This means there is hope that you can get better.
Feeling the pain can become a habit as proved by neuroscience.
Neural circuits that fire repeatedly become more sensitive and hyperactive.
They can even get bigger and stronger—like a muscle does when you work out.
Pain can be triggered by a structural disorder or simply the neural
pathways in the brain.
A significant proportion of pain that we experience is brain-induced.
MRI findings often do not correlate with the individual experience of pain.
We can make this distinction between structural pain and nonstructural pain—sometimes it’s a combination of the two.
The Missing Piece of my Back Pain Story
The emotional pain of my inner conflicts eventually manifested as physical pain.
How can you expect your body to be healthy when your mental health is in tatters?
I experienced terrible back pain when I was under extreme stress or anxiety due to major changes in my life.
It was almost easier to deal with the back pain than to quit my job, say no to the £££, disappoint everyone else around me with my “career suicide” decisions.
The pain often appeared after stressful periods as if it was trying to protect me from putting myself in another stressful situation.
It’s not Science; It’s Common Sense
If your herniated disc is indeed herniated, it should be herniated 24/7 and pressing against that nerve the whole time.
But how come you have moments when you don’t feel any pain?
How come you sometimes forget the pain?
Does the disc go like, “OK, I’ve given them enough pain for the day, I’ll come back tomorrow. You know… I don’t feel like pressing their nerve today”.
I’m sure that if you saw a tiger in front of you right now, you’d run faster than Usain Bolt and you’d forget your back pain until you’d get back to safety.
It’s strange and incomprehensible, I know.
But when you have a headache or a migraine or some other sort of pain in your body, you don’t go to have an MRI the next morning being almost sure that some part of your body is damaged and might require surgery.
But when it comes to back pain, we all self-diagnose ourselves.
We don’t even have to go to the GP.
Oh, my back is probably damaged, I need medication, an MRI, and probably injections or surgery if it gets worse.
If you’re still sceptical, I totally understand.
This is a entirely new paradigm and paradigms don’t shift easily.
As Sherlock Holmes said, “There’s nothing more deceptive than an obvious fact”.
But with the advancement of neuroscience, we’ll manage to understand the brain, that is still a mystery to scientists, better.
It took people time to believe that the world is not flat.
As Donald James Wheal said:
A truth’s initial commotion is directly proportional to how deeply the lie was believed. It wasn’t the world being round that agitated people, but that the world wasn’t flat. When a well-packaged web of lies has been sold gradually to the masses over generations, the truth will seem utterly preposterous and its speaker raving lunatic. – Donald James Wheal (1931-2008)
How Do I Get Relief from my Back Pain Then?
I use a series of techniques to help my clients get rid of their chronic pain but I’d start with one simple exercise.
For the next two weeks, practice the “No Salvation” exercise.
Give up on the pain, the anger, the desperation and anything else you feel.
Don’t fight the pain. Don’t try to control the pain. Don’t anticipate the pain. Don’t check in with the pain.
Welcome all of the racing thoughts too.
If you want to shout, shout. If you want to cry, cry.
If you want to tell me to f*** off, I’ll not get offended.
But live your life for the next two weeks as if there is no cure for you.
Pretend you’ve failed.
Pretend you’ll live the rest of your life in pain with zero chances of getting relief.
Go for a walk while in pain. Go to work while in pain. Watch a film, make a carrot cake, even start to dance slowly!
Because remember, there is no cure.
Pretend all is over.
You’ve married your condition whatever it is and you can’t divorce it!
You will notice amazing things will happen…
What keeps the pain there is the fear of it.
You may believe that the pain has to go away so that you can get your life back.
However, it’s the opposite.
You start living your life again and then you see your pain disappear.
With love, Angelos
P.S. Subscribe to receive my tips on chronic pain relief straight to your inbox.
P.P.S Want to learn more about how repressed emotions cause physical pain and how to get rid of your pain? Read my guide on the Tension Myositis Syndrome (TMS).

5 replies on “Chronic Back Pain – The Lies and the Truth”
A real eye opener. Will follow your advice for two weeks, but if I think about my pain then your reasons makes sence. Also, my mom went for two back operations, neck and both hips and she is less mobile than before all those operations. Thank you
Thank you Mandie. I wish you and your mom well.
I will give it a try Angelos, but I feel so down at the moment, I guess it is going to be tough getting out of the victim mode? Thanks for the good advice. Fred
I do believe you are right in your description of how to relieve your pain. The difficult part is having the courage and will to be able to see those two weeks through without losing your way yet time and time again. How do you conquer that?
Fred, I totally understand. I’d like to invite you to see it from a different perspective. What if you didn’t need any courage or will this time? What if you truly gave up? What if you stopped any effort to control pain? Truly surrendering. It will not be easy to get out of the habit of being hyper-vigilant or thinking constantly about pain. But once this happens, relax. Pretend all is over. No more “babying” your back. You can now move without restrictions, sit down on the floor, sleep in any position. It’s liberating to consider yourself defeated. There is no expectation any more. There is nothing wrong you could do. Managing pain is a full-time job. What if you took a 2-week holiday? Be well, Angelos